
CHIP
Children in Texas without health insurance may be able to get low-cost or free health coverage from the Children’s Health Insurance Program (CHIP). Community First Health Plans is the only non-profit, locally owned health plan available in our service area that offers the CHIP program.
About CHIP
CHIP is designed to cover children in families that earn too much money to qualify for Medicaid but cannot afford to buy private insurance.
This program covers doctor visits, prescription drugs, dental care, eye exams, glasses, and more.
Benefits & Services
CHIP covers services needed to keep you healthy, including:
- Regular checkups with the doctor and dentist.
- Prescription drugs and vaccines.
- Hospital care and services.
- X-rays and lab tests.
- Vision and hearing care.
- Access to medical specialists and mental health care.
- Treatment of special health needs and pre-existing conditions.

Need a printed Member Handbook?
The CHIP Member Handbook is available to you in print, free of charge, and mailed within five business days. For your free copy, please call 1-800-434-2347 or make a request through your secure Member Portal.
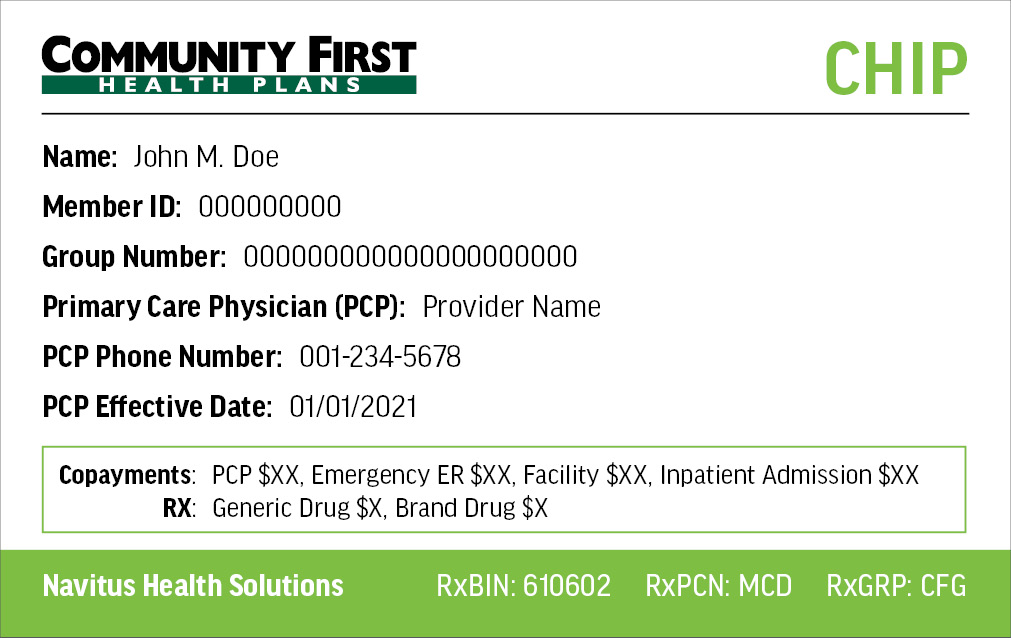
Need a replacement ID card?
To replace a lost or stolen Member ID card, log in to your Member Portal. Once you have logged into your Member Portal account, use the drop-down for My Health Plan and select “ID Card Request” to order a new ID card.
Requirements
In order to be eligible for CHIP, a child must be:
- Under 19 years of age,
- Uninsured (determined ineligible for Medicaid, and not covered through a group health plan or creditable health insurance),
- A citizen or meet immigration requirements,
- A resident of the state, and
- Eligible within the state’s CHIP income range, based on family income, and any other state specified rules in the CHIP state plan.
Processes
Dedicated to the health and well-being of our Members, Community First Health Plans has developed guidelines to ensure your safety and protect your rights. Learn more about our processes and policies below.
As a CHIP Community First Health Plans Member, you have certain rights and responsibilities. To view your rights and responsibilities, click here. You can also find your rights and responsibilities in the CHIP Member Handbook.
Community First might deny a health care service or medicine if it is not medically necessary. A medicine can also be denied if the medicine does not work better than other medicines on the Community First Preferred Drug List; or if there is another medicine that is similar that you must try first that you have not used before.
If you disagree with the denial, you can ask for an appeal.
To learn more about our appeals process, click here.
If you receive benefits through Medicaid’s CHIP Program, contact Community First Health Plans toll-free at 1-800-434-2347 or locally at 210-358-6300 to file a complaint first. Once you have gone through our complaint process you can file a complaint to TDI. This information can also be found in your Member Handbook. To learn more about our complaint process, click here.
The Community First Health Plans Notice of Privacy Practices describes how medical information about the member may be used and disclosed and how the member can get access to this information. To learn more about our privacy policy, click here.


