
STAR Kids
STAR Kids is a Texas Medicaid program that provides Medicaid benefits to children and adults 20 and younger who have disabilities. Community First Health Plans is the only non-profit, locally owned health plan available in our service area that offers the STAR Kids program.
About STAR Kids
STAR Kids is designed to meet the unique needs of youth and children with disabilities.
Community First Health Plans provides Service Coordination for our STAR Kids Members. Service Coordination helps identify needs and connects Members to services and providers.
Community First Service Coordinators:
- Review each Member’s specific needs.
- Help the family and health plan create a unique individual service plan for each Member.
- Perform the STAR Kids Screening and Assessment (SK-SAI), a standard screening and assessment process health plans use to determine each child’s needs as they relate to health and independent living.
Benefits & Services
STAR Kids covers services needed to keep you healthy, including:
- Prescription drugs
- Hospital care
- Primary and specialty care
- Preventive care
- Personal care services
- Private duty nursing
- Durable medical equipment and supplies

Need a printed Member Handbook?
The STAR Kids Member Handbook is available to you in print, free of charge, and mailed within five business days. For your free copy, please call 1-855-607-7827or make a request through your secure Member Portal.
For more information about how your health plan works, please read the STAR Kids Member Handbook.
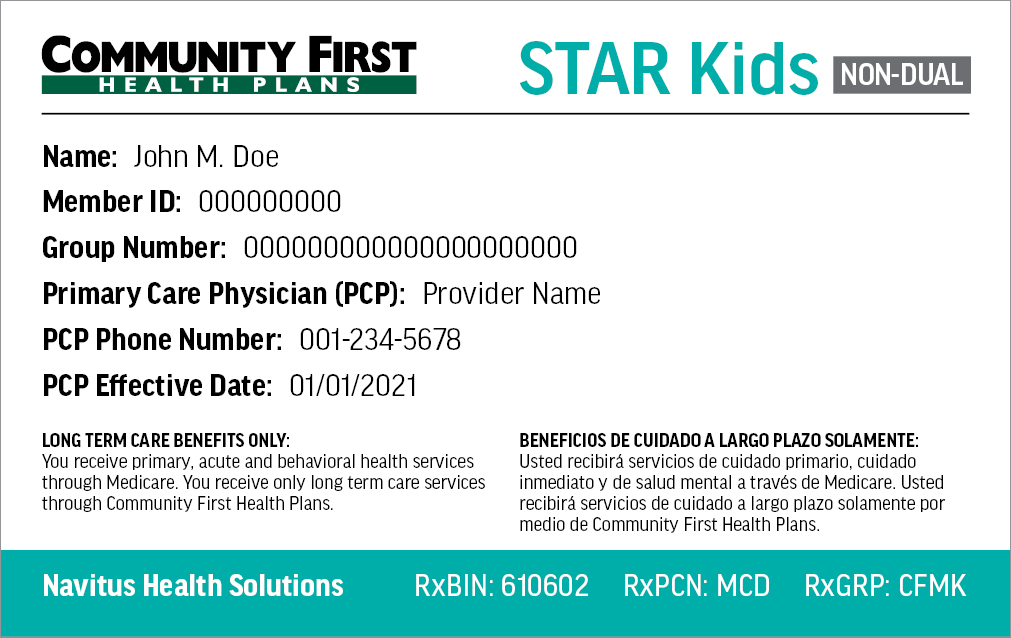
Need a replacement ID card?
To replace a lost or stolen Member ID card, log in to your Member Portal. Once you have logged into your Member Portal account, use the drop-down for My Health Plan and select “ID Card Request” to order a new ID card.
Requirements
To qualify for STAR Kids, your child must be 20 or younger, covered by Medicaid, and meet at least one of the following:
- Receive Supplemental Security Income (SSI)
- Receive SSI and Medicare
- Receive services through the Medically Dependent Children Program (MDCP) waiver
- Receive services through the Youth Empowerment Services (YES) waiver
- Live in a community-based intermediate care facility for individuals with an intellectual disability or related condition (ICF/IID) or nursing facility
- Receive services through a Medicaid Buy-In program
- Receive services through any of the following Department of Aging and Disability Services (DADS) intellectual and developmental disability (IDD) waiver programs:
- Community Living Assistance and Support Services (CLASS)
- Deaf Blind with Multiple Disabilities (DBMD)
- Home and Community-based services
- Texas Home Living (TxHmL)
Processes
Dedicated to the health and well-being of our Members, Community First Health Plans has developed guidelines to ensure your safety and protect your rights. Learn more about our processes and policies below.
- Rights & Responsibilities
- Appeals Process
- Complaint Process
- State Fair Hearing & External Medical Review Process
- Privacy Policy
As a Community First STAR Kids Member, you have certain rights and responsibilities. To view your rights and responsibilities, click here. You can also find your rights and responsibilities in the STAR Kids Member Handbook.
Community First might deny a health care service or medicine if it is not medically necessary. A medicine can also be denied if the medicine does not work better than other medicines on the Community First Preferred Drug List; or if there is another medicine that is similar that you must try first that you have not used before.
If you disagree with the denial, you can ask for an appeal.
To learn more about our appeals process, click here.
If you receive benefits through Medicaid’s STAR Kids Program, contact Community First Health Plans toll-free at 1-855-607-7827 or locally at 210-358-6403 to file a complaint first. Once you have gone through our complaint process you can file a complaint to HHSC. This information can also be found in your Member Handbook. To learn more about our complaint process, click here.
A State Fair Hearing is when the Texas Health and Human Services Commission (HHSC) directly reviews our decisions with your medical care.
If you ask for a State Fair Hearing, you can also ask for an External Medical Review where independent health care experts review your request to receive services. This review is an optional, extra step you can take to get your case reviewed for free before your State Fair Hearing. It doesn’t change your right to a State Fair Hearing.
To learn more about requesting a State fair Hearing and External Medical Review, click here.
The Community First Health Plans Notice of Privacy Practices describes how medical information about the member may be used and disclosed and how the member can get access to this information. To learn more about our privacy policy, click here.



