STAR Medicaid
STAR Medicaid provides no-cost health coverage for low-income children, pregnant women, and families in Texas. Community First Health Plans is proud to be the only local, non-profit health plan that offers STAR Medicaid in our service area.
About STAR Medicaid
STAR Medicaid is designed to meet the unique needs of low-income children, pregnant women, and families.
Community First Health Plans provides Service Management for STAR Members with special health care needs. Service Management can help ensure you get the health care services you need and other services that might not be covered by your health plan like food, housing, personal care services, and special programs like Community First Choice.
Special health care needs that may qualify for Service Management include:
- Serious, ongoing illnesses;
- Chronic or complex conditions;
- Disabilities; and
- Conditions that require therapeutic intervention and evaluation by appropriately trained staff.
Benefits & Services
STAR Medicaid covers services needed to keep you/your child healthy, including:
- Regular checkups at the doctor and dentist
- Prescription drugs and vaccines
- Hospital care and services
- X-rays and lab tests
- Vision and hearing care
- Access to medical specialists and mental health care
- Treatment of special health needs
- Treatment of pre-existing conditions
Families/children who get STAR Medicaid do not pay for medical services or prescription benefits.

Need a printed Member Handbook?
The STAR Medicaid Member Handbook is available to you in print, free of charge, and mailed within five business days. For your free copy, please call 1-800-434-2347 or make a request through your secure Member Portal.
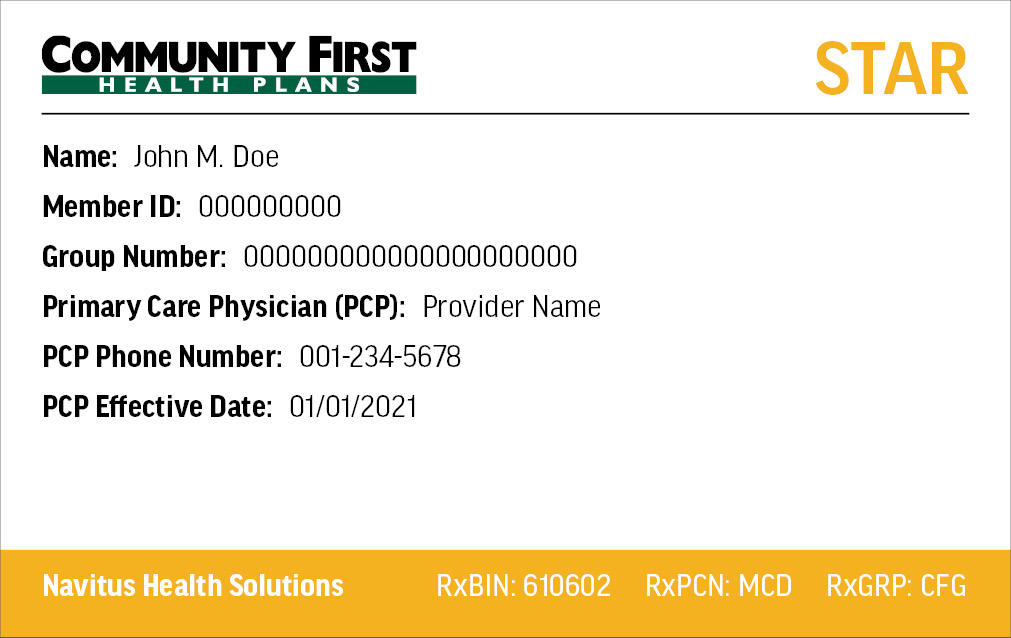
Need a replacement ID card?
To replace a lost or stolen Member ID card, log in to your Member Portal. Once you have logged into your Member Portal account, use the drop-down for My Health Plan and select “ID Card Request” to order a new ID card.
Requirements
To qualify for STAR Medicaid, you must be a Texas Resident and a U.S. citizen or non-qualified citizen. STAR Medicaid covers low-income children, pregnant women and families.
Processes
Dedicated to the health and well-being of our Members, Community First Health Plans has developed guidelines to ensure your safety and protect your rights. Learn more about our processes and policies below.
- Rights & Responsibilities
- Appeals Process
- Complaint Process
- State Fair Hearing & External Medical Review Process
- Privacy Policy
As a STAR Medicaid Community First Health Plans Member, you have certain rights and responsibilities. You can also find your rights and responsibilities in the STAR Medcaid Member Handbook. To view the document, click here.
Community First might deny a health care service or medicine if it is not medically necessary. A medicine can also be denied if the medicine does not work better than other medicines on the Community First Preferred Drug List; or if there is another medicine that is similar that you must try first that you have not used before.
If you disagree with the denial, you can ask for an appeal.
To learn more about our appeals process, click here.
If you receive benefits through Medicaid’s STAR Program, contact Community First Health Plans toll-free at 1-800-434-2347 or locally at 210-358-6060 to file a complaint first. Once you have gone through our complaint process you can file a complaint to HHSC. This information can also be found in your Member Handbook. To learn more about our complaint process, click here.
A State Fair Hearing is when the Texas Health and Human Services Commission (HHSC) directly reviews our decisions with your medical care.
If you ask for a State Fair Hearing, you can also ask for an External Medical Review where independent health care experts review your request to receive services. This review is an optional, extra step you can take to get your case reviewed for free before your State Fair Hearing. It doesn’t change your right to a State Fair Hearing.
To learn more about requesting a State fair Hearing and External Medical Review, click here.
The Community First Health Plans Notice of Privacy Practices describes how medical information about the member may be used and disclosed and how the member can get access to this information. To learn more about our privacy policy, click here.


