
STAR+PLUS
STAR+PLUS is a Texas Medicaid-managed care program for adults who have disabilities or are age 65 or older. Community First Health Plans is the only non-profit, locally owned health plan available in our service area that offers the STAR+PLUS program.
About STAR+PLUS
STAR+PLUS is designed to meet the unique needs of adults who have disabilities or are age 65 or older.
Community First Health Plans provides Service Coordination for our STAR+PLUS Members. Service Coordination helps identify needs and connects Members to services and providers.
Community First Service Coordinators:
- Review each Member’s specific needs.
- Help the family and health plan create a unique individual service plan for each Member.
- Assist the member to get the medical and long-term services and support they need as they relate to health and independent living.
Benefits & Services
STAR+PLUS covers services needed to keep you healthy, including:
- Prescription drugs
- Hospital care
- Primary and specialty care
- Preventive care
- Personal care services
- Skilled nursing
- Durable medical equipment and supplies

STAR+PLUS Dual Members (Members who have Medicare) are not required to choose a Primary Care Provider (PCP) because dual-eligible Members receive acute care from their Medicare providers. Under the STAR+PLUS program, Community First provides Medicaid Long Term Services & Supports (LTSS) to dual-eligible Members. Community First recommends choosing a PCP to assist Members in coordinating care. No PCP information will appear on the STAR+PLUS Dual member ID card.
Need a physical Member Handbook?
The STAR+PLUS Member Handbook is available to you in print, free of charge, and mailed within five business days. For your free copy, please call 1-855-607-7827 or make a request through your secure Member Portal.
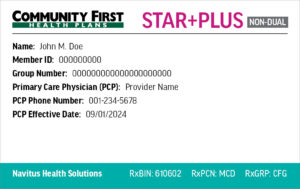
Need a replacement ID card?
To replace a lost or stolen Member ID card, log in to your Member Portal. Once you have logged into your Member Portal account, use the drop-down for My Health Plan and select “ID Card Request” to order a new ID card.
Requirements
To qualify for STAR+PLUS, you must be approved for Medicaid and meet at least one of the following:
- Age 21 or older, getting Supplemental Security Income (SSI) benefits and able to get Medicaid due to low income.
- Not getting SSI and need the type of services in STAR+PLUS HOME and Community-Based Services.
- Age 21 or older, getting Medicaid through what are called “Social Security Exclusion programs” and meet program rules for income and asset levels.
- Age 21 or over residing in a nursing home and receiving Medicaid while in the nursing home.
- In the Medicaid for Breast and Cervical Cancer program.
Processes
Dedicated to the health and well-being of our Members, Community First Health Plans has developed guidelines to ensure your safety and protect your rights. Learn more about our processes and policies below.
- Rights & Responsibilities
- Appeals Process
- Complaint Process
- State Fair Hearing & External Medical Review Process
- Privacy Policy
As a STAR+PLUS Community First Health Plans Member, you have certain rights and responsibilities. You can also find your rights and responsibilities in the STAR+PLUS Member Handbook. To view the document, click here.
Community First might deny a health care service or medicine if it is not medically necessary. A medicine can also be denied if the medicine does not work better than other medicines on the Community First Preferred Drug List; or if there is another medicine that is similar that you must try first that you have not used before.
If you disagree with the denial, you can ask for an appeal.
To learn more about our appeals process, click here.
If you receive benefits through Medicaid’s STAR+PLUS Program, call your medical or dental plan first. If you don’t get the help you need there, you should do one of the following:
- Call Medicaid Managed Care Helpline at 1-866-566-8989 (toll-free).
- Online: https://hhs.texas.gov/about-hhs/your-rights/hhs-office-ombudsman
- Mail: Texas Health and Human Services Commission
Ombudsman Managed Care Assistance Team
P.O. Box 13247
Austin, TX 78711-3247 - Fax: 1-888-780-8099 (toll-free).
A State Fair Hearing is when the Texas Health and Human Services Commission (HHSC) directly reviews our decisions with your medical care.
If you ask for a State Fair Hearing, you can also ask for an External Medical Review where independent health care experts review your request to receive services. This review is an optional, extra step you can take to get your case reviewed for free before your State Fair Hearing. It doesn’t change your right to a State Fair Hearing.
To learn more about requesting a State fair Hearing and External Medical Review, click here.
The Community First Health Plans Notice of Privacy Practices describes how medical information about the member may be used and disclosed and how the member can get access to this information. To learn more about our privacy policy, click here.


