On January 1, 2023, HHSC will designate one medication as the primary preferred direct-acting antiviral (DAA) drug option for treating Hepatitis C infection. HHSC will designate all other DAA drugs on the Medicaid formulary as non-preferred.
All Medicaid clients are eligible for DAA treatment with the primary preferred agent regardless of the client’s METAVIR fibrosis score, and prior authorization is not required. Any enrolled Medicaid provider can prescribe the preferred drug, and a drug screening is not required. Prescribers are allowed to write prescriptions for the entire course of therapy, so clients will no longer need to request additional refills throughout their treatment duration. Prescribers may choose to write a prescription for the entire treatment cycle or have the client return for further testing if warranted. Drugs identified on the preferred drug list (PDL) as preferred are available without prior authorization. The table below summarizes the national drug codes (NDCs) impacted by this:
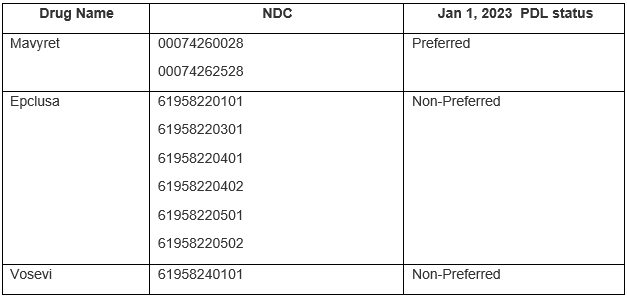
HHSC will publish an update to the Texas Medicaid Preferred Drug List (PDL) on January 1, 2023, to designate preferred and non-preferred options for DAA treatment. HHSC will include the changes in the daily PDL file delivered to managed care plans via TXMedconnect by December 15. PDL statuses will be future-dated to reflect the January 1 changes.
The PDL status for all other non-preferred DAA drugs currently on the formulary will not change. For any non-preferred DAA drugs, HHSC will continue to apply PDL prior authorization criteria for all Medicaid clients, both fee-for-service and managed care. Additionally, effective January 1, the following clinical prior authorization forms for Hepatitis C treatment agents will be retired and no longer necessary:
● Antiviral Agents for Hepatitis C Virus – Initial Request (HHS Form 1335)
● Antiviral Agents for Hepatitis C Virus – Initial Request – Addendum (HHS Form 1342)
Contact:
Email ProviderRelations@cfhp.com or call 210-358-6294.

