Community First will not be requiring authorization for behavioral health services that are managed by and billed by the patient’s PCP. This is part of the Collaborative Care Model (CoCM).
Senate Bill 672, 87th Legislature, Regular Session, 2021 directed HHSC to provide medical assistance reimbursement to a treating health care provider who participates in Medicaid for the provision to a child or adult medical assistance recipient of behavioral health services that are classified by a Current Procedural Terminology (CPT) code as collaborative care management services. In response to this requirement, Medical and Dental Benefits staff drafted a new Medicaid medical policy for the Collaborative Care Model (CoCM) services that includes coverage for four related CPT codes.
Effective for dates of service on or after June 1, 2022, Community First will not require an authorization for behavioral health services that are managed by and billed by the member’s PCP, according to the Collaborative Care Model (CoCM).
The CoCM is a systematic approach to the treatment of behavioral health conditions (mental health or substance use) in primary care settings. The model integrates the services of behavioral health care managers (BHCMs) and psychiatric consultants with PCP oversight to proactively manage behavioral health conditions as chronic diseases.
CoCM services must be provided under the direction of the PCP and are benefits when provided in an office, outpatient hospital, inpatient hospital, skilled nursing facility or intermediate care facility, extended care facility, and “other location” settings.
CoCM services are individually delivered, time-based, monthly services that include the following:
- Outreach and engagement
- Completing an initial assessment
- Developing an individualized and person-centered plan of care
- Providing brief interventions and other focused treatments
- Conducting weekly caseload reviews with the psychiatric consultant
- Monitoring and tracking a person’s progress using a registry
Only the PCP may submit claims for CoCM services. The BHCM and psychiatric consultant are reimbursed by the PCP via a contract, employment, or other arrangement.
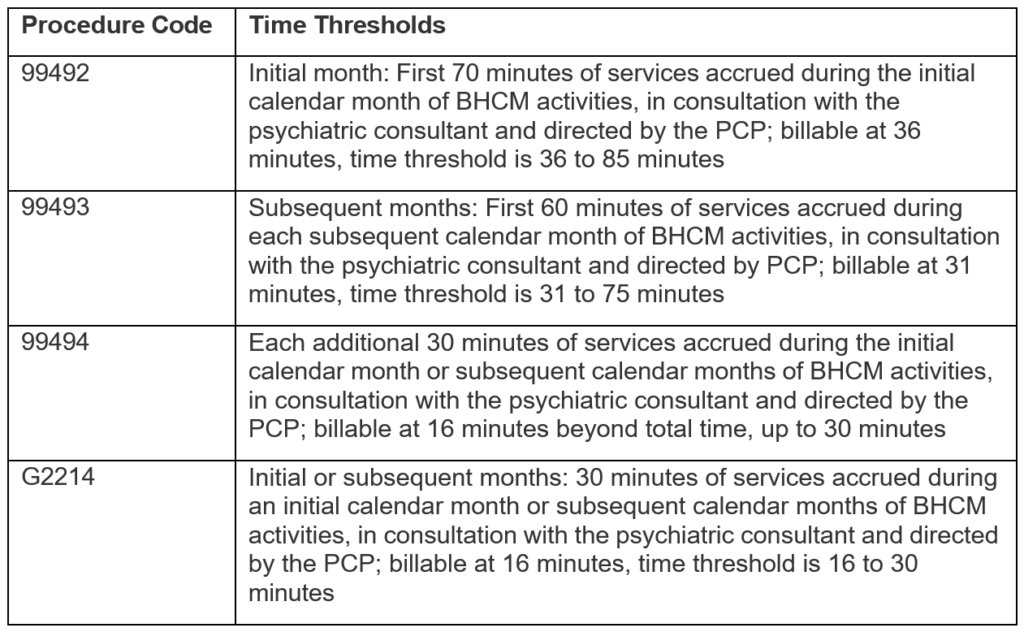
Effective June 1, 2022, the PCP must submit the following procedure codes and meet the designated time thresholds to bill for monthly CoCM services in all settings:
The CoCM only applies to behavioral health services that are managed by and billed by the member’s PCP. Community First will not be requiring an authorization for these service when they are being managed by and billed by the member’s PCP.
Information about the benefit will be published in the Medical and Nursing Specialists, Physicians, and Physician Assistants Handbook (Vol. 2, Provider Handbooks) in the Texas Medicaid Provider Procedure Manual.
To ensure providers have an established CoCM program, HHSC is developing an attestation form that fee-for-service providers will have to sign prior to the delivery of CoCM
services. Providers will need to attest that they are actively providing care consistent with the CoCM’s core principles and specific function requirements, i.e., patient-centered care, team structure with identified staff, measurement-based treatment using validated tools, and accountable care using a registry, as described in the CoCM Medicaid medical policy. The form will be available at a future date for MCOs to use, or edit, as needed.
For more information on registry requirements, refer to Advancing Integrated Mental Health Solutions (AIMS) Center, University of Washington, Psychiatry and Behavioral Sciences Division of Population Health.
For more information on payment for CoCM in primary care, refer to the American Medical Association’s webinar titled Experts on practical billing strategies for the collaborative care model.
For additional information, please contact Provider Relations at (210) 358-6294 or ProviderRelations@CFHP.com.

