Key Details:
Texas Medicaid managed care organizations (MCOs) must provide all medically necessary, Medicaid-covered services to Medicaid members who are enrolled in their MCO. Administrative procedures, such as prior authorization, precertification, referrals, and claims and encounter data filing, may differ from traditional Medicaid (fee-for-service) and from MCO to MCO. Providers should contact the member’s specific MCO for details.
Effective for dates of service on or after December 1, 2024, certain non-surgical services procedure codes will no longer be reimbursed separately for hospital-based ambulatory surgery centers (HASC) and ambulatory surgery centers (ASC) because they are included in the Medicare ASC global payment. This change applies to Texas Medicaid and the Children with Special Health Care Needs (CSHCN) Services Program.
The following non-surgical services procedure codes will be affected under this change:
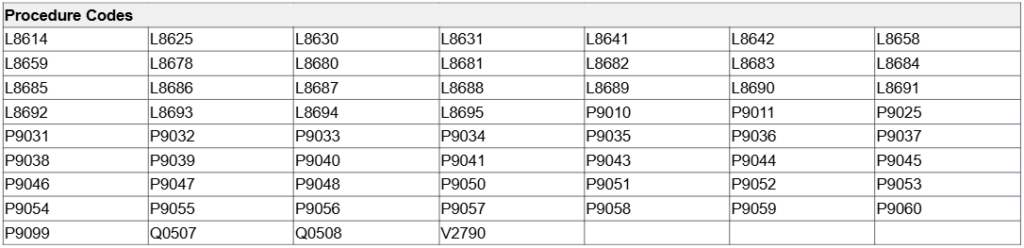
The HASC’s and ASC’s Static Fee schedule will be updated to reflect these changes.
For more information, call the TMHP Contact Center at 800-925-9126 or the TMHP-CSHCN Services Program Contact Center at 800-568-2413.
Providers are encouraged to share this information with their staff. If you have any questions about this notice, please email Provider Relations at ProviderRelations@cfhp.com or call 210-358-6294. You can also contact your Provider Relations Representative directly.
To access all Provider alerts:
- Log into the Community First Provider Portal
- Go to CommunityFirstHealthPlans.com/Provider-News
- Sign up for the Community First Provider eNewsletter

