Effective August 1, 2024, the Attestation Form for the Collaborative Care Model (CoCM) in Texas Medicaid will be removed from the Texas Medicaid & Healthcare Partnership (TMHP) website and made available in the Provider Enrollment and Management System (PEMS).
Key Details:
Prior to delivering CoCM services, applicable providers will be required to complete the CoCM attestation form in PEMS to confirm that they have an established CoCM program and that they are actively providing CoCM services consistent with the model’s core principles and specific functional requirements.
Note: The attestation form will not be available in PEMS before August 1, 2024. Also, providers that completed the CoCM attestation form previously will be required to complete the new CoCM attestation form in their PEMS enrollment record. The previous attestation will no longer be active as of August 1, 2024.
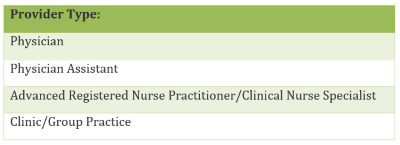
The following provider types will be subject to CoCM attestations:
Enrolled providers that do not have an in-flight enrollment application that is pending approval have a grace period of 60 days to attest their CoCM status in PEMS by using the Maintenance Practice Location – Attestation request type. Providers can only add the CoCM attestation through this request type and cannot make changes to other information in their enrollment record or to their existing enrollment. If providers do not attest within the 60-day grace period, reimbursement for CoCM services will be denied.
Providers that have in-flight (existing, re-enrollment, or revalidation) enrollment requests that were submitted before August 1, 2024, and are pending approval after August 1, 2024, may be subject to an enrollment deficiency review. Provider Enrollment may send the application back to the provider to select either Yes or No to the CoCM attestation question in the new “Collaborative Care Model (CoCM) Services” section. This section is found on the Program and Service Participation Details page in PEMS.
Note: The provider must answer the CoCM attestation question for each enrolled Acute Care practice location. The question is not required for disenrolled or disenrolling locations. Once providers have attested, they will be required to re-attest upon revalidation of their enrollment record.
Adding or Terminating a CoCM Attestation:
Providers can add or terminate their CoCM attestation through the new PEMS Maintenance Practice Location – Attestation request type.
Once a CoCM attestation is on file, a provider may terminate their attestation for a practice location by selecting No to the CoCM attestation question in PEMS using the Maintenance Practice Location – Attestation request type. This action will disassociate the CoCM attestation from that location.
The provider must repeat this action for each practice location at which they no longer provide CoCM services.
For additional information, refer to the Texas Medicaid Provider Procedures Manual (TMPPM), Medical and Nursing Specialists, Physicians, and Physician Assistants Handbook, section 9.3, “Collaborative Care Model (CoCM).”
About PEMS:
PEMS is the single tool for provider enrollment, re-enrollment, revalidation, change of ownership, and maintenance requests (maintaining and updating provider enrollment record information). PEMS has automated and streamlined the process for provider ease of access by removing the requirement to use paper forms.
For more information, call the TMHP Contact Center at 800-925-9126
Resources:
· For more information about the new CoCM attestation process, refer to the provider notification at Collaborative Care Model Attestation Process to Update on August 1, 2024.
· For information about the CoCM Medicaid benefit, refer to Section 9.3 of the Medical and Nursing Specialists, Physicians, and Physician Assistants Handbook (Vol. 2, Provider Handbooks) in the TMPPM.
· For more information on the CoCM to include evidence base, core principles and team structure, refer to Advancing Integrated Mental Health Solutions (AIMS) Center, University of Washington, Psychiatry and Behavioral Sciences Division of Population Health.
Next steps for Providers:
Providers should share this communication with their staff.
Community First Resources:
https://communityfirsthealthplans.com/provider-newsletter
https://communityfirsthealthplans.com/providers/
Contact:
Email ProviderRelations@cfhp.com or call 210-358-6294.

